Europe is suffering from a healthcare crisis, with chronic staff shortages, low pay and overtime prompting strikes in Germany, Slovenia, and Sweden. In France meanwhile, a controversial medicine education reform has students and doctors up in arms.
Hospitals across Europe appear to be on life support.
Whether it's in France, Slovenia or Sweden, hospitals are facing staff shortages, lower wages and increasing levels of overtime, prompting industrial action across the healthcare sector which inevitably impacts patient care.
In Sweden, healthcare workers went on strike for the first time in 16 years to protest against their working hours and low pay over 78 consecutive days in 2024.
It's less common to see strikes in the Nordic countries than in other parts of Europe, yet after four months of collective bargaining negotiations, the Swedish Association of Health Professionals' hand was forced, and it went on strike from 11 April to 28 June.
"We met a dead end in the negotiations," said Sineva Ribeiro, president of the Swedish Association of Health Professionals, a trade union with a membership of 114,000 representing nurses, midwives, biomedical scientists and radiographers. "We had to go on strike. We had to have a conflict.”
The trade union also issued an overtime ban. "In 2023, they [members of the association] did three million overtime hours," Ribeiro said. "So we knew that there was a lack of nurses, midwives, radiographs and X-ray nurses."
In the end, the Swedish Association of Health Professionals managed to obtain reduced working hours for 10% of its members — those who work night shifts — a 3.05% salary increase and an agreement that employers pay for nurse specialisations.
On the flipside, they agreed to abandon calls to reduce medical staff's weekly working hours from 40 to 37.
More generally, deteriorating working conditions are said to be one of the main factors forcing health workers out of Sweden and into neighbouring countries.
"We have about 20,000 nurses working in Norway because they pay more and they have less hours a week", Ribeiro said.
In addition, 13,000 qualified nurses have left the profession, leaving a taxpayer-funded black hole of more than €60 million, according to a report by the Swedish National Health Competence Council published in June.
"It is better [in Sweden] maybe than other EU countries," said Ribeiro. "But we still have a big lack of nurses who may treat the health of the population. And we never know when the next pandemic can come."
'A ticking time bomb'
But the reality is that there's a similar problem across the EU.
Public hospitals in countries around the bloc are confronted with parallel challenges, including an ageing population who will need more healthcare and difficulty in replacing healthcare workers who retire because the profession is not as attractive as it used to be.
"There is an increase of demand, basically because of four main factors the aging of the population, the increase of multimorbidity and chronic conditions, the backlogs accumulated during the COVID-19 pandemic in terms of waiting list, and also because of increased expectations of patients", explained Tomas Zapata, regional advisor on health workforce and service delivery at the World Health Organization (WHO) Europe.
He told Euronews that European countries' health sectors are facing a "workforce crisis", highlighted by the strikes by different types of healthcare professionals.
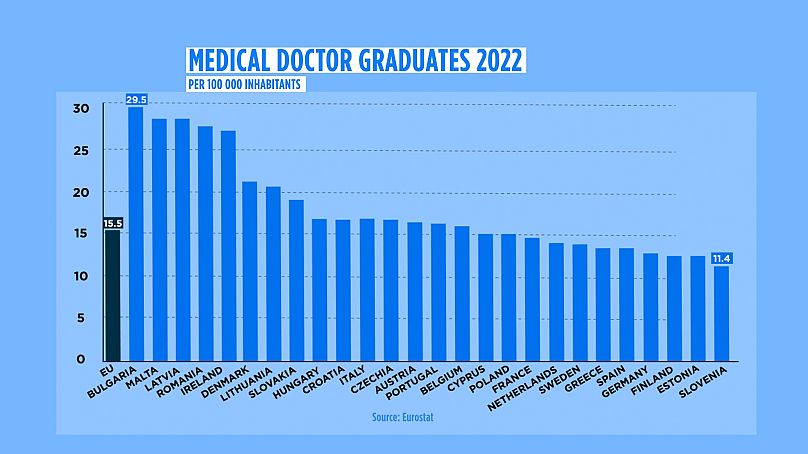
"We have more doctors and nurses than ever. So in the last 10 years, there has been a 20% increase of doctors in the whole region and a 10% increase in the number of nurses. However, the demand is growing at a faster pace. So that means that we are having this shortage, this gap between the demand and the availability of health workers", he said.
A regional report published by the World Health Organization (WHO) Europe in September 2022 warned of a "ticking timebomb" threatening health systems in Europe and Central Asia.
It said that one of the main challenges is the ageing health and care workforce, noting that 40% of doctors in 13 of the 44 countries it looked at are already aged 55 or older.
The report also highlights poor mental health among those in the medical profession affected by long working hours, inadequate professional support, and serious staff shortages.
In some countries, over 80% of nurses reported some form of psychological distress caused by the COVID-19 pandemic. As many as nine out of 10 nurses were thinking of quitting their jobs, according to the report.
All of these issues are forcing doctors and other healthcare workers across Europe into strikes, in an effort for better working conditions.
Germany demands 'top-notch' care
In January, thousands of doctors at state-owned university hospitals in Germany staged a strike after collective bargaining talks with hospital managers failed.
Some 5,000 doctors joined a "warning strike", organised by the Marburger Bund in the northern city of Hanover, the trade union said.
It demanded a 12.5% pay rise and higher bonuses for working nights, weekends and public holidays for 20,000 doctors in university hospitals.
They took to the streets again in March after the fourth round of negotiations with the 16 federal states (Länder) which run public hospitals, ended in failure. According to the Marburger Bund, approximately 7,000 doctors from 23 institutions across Germany took part in various demonstrations this time around.
"We cannot accept that university medicine remains the last wheel of the wagon in terms of doctors' salaries", Andreas Botzlar, second chairman of the Marburger Bund, said in a statement.
"The recent round of negotiations has left us with the impression that the Länder still do not understand what it is all about: we are demanding fair conditions for top-notch medicine. Not more — but also not less," he added.
Slovenia sees longest-ever doctors' strike
Doctors and dentists working in the Slovenian public healthcare service went on strike in January, in what has become the country's longest-ever doctors' strike.
They withdrew their consent for overtime work in a bid to pressure the government into honouring its commitments to a previously tabled health reform and bringing it back to the negotiating table.
In 2023, Fides, the doctors and dentists trade union, signed an agreement with the government to create a separate pay pillar in the public sector payscale for healthcare professionals, but this never came to fruition.
"Employees are leaving public institutions, and good paediatricians are being penalised for their willingness to help the public sector," Damjan Polh, Fides president, said in a statement. "Promises about reforms remain unfulfilled, and laws in the field of healthcare are written by those who do not understand it at all."
The government adopted a proposal to amend the Medical Services Act, which would establish a minimum working time requirement during a strike "to guarantee the stable operation of the healthcare system".
Fides has appealed to Slovenia's Constitutional Court to question such a measure's constitutionality and legality. According to the union, it would "further restrict the right of doctors to strike".
Most recently, the trade union informed the Slovenian government in August of additional strike demands to protect the medical profession.
Controversial reform in France
Over in France, a measure of a different kind has sparked outrage among medical students: there will be 1,510 fewer openings for junior doctors this autumn.
Only 7,974 positions will have been opened this year, compared to 9,484 in 2023, according to official government data from July.
In France, junior doctors, or "internes en médecine", are medical students who have completed their sixth year of study out of 12. They work full-time at a hospital or in another medical institution under the supervision of a senior while continuing their studies.
"We are all very scared (...) The work in hospitals is very difficult, it is very demanding mentally and physically for junior doctors," said Marie, who is finishing her sixth year of medical studies. "And now there will be fewer of us in the autumn while the workload won't diminish."
According to the government, the number of positions was reduced because the number of candidates who took part in the competitive entry exams to win the placements also fell.
The figures have raised eyebrows among trade unions, however.
"Every year, there is an adaptation of the position openings depending on the number of junior doctors who run," said Dr Agnès Ricard Hibon, spokesperson for the trade union SAMU Urgences de France. "Except that in this case, there have been way more people redoing the year."
Medical specialisations will suffer to different degrees: general medicine and ophthalmology positions are due to fall by 18%, while there will be 15% fewer openings in emergency medicine.
"There are some disciplines like plastic surgery, which are more impacted. Others are preserved such as pediatrics or pediatric surgery because there is a huge need", Hibon said.
Yet some students claim many of their classmates chose to repeat their year and failed their exams on purpose, as they were the first cohort to sit the placement entry exams which were brought in by a contested medical studies reform in 2020. They claimed they didn't want to be a "crash test" cohort.
Nevertheless, Hibon said the decrease in the number of junior doctors shouldn't have a major impact on hospitals: "They are systematically supervised by senior doctors. They are not the ones who run the services," she said.
On the other hand, some students have launched a petition online asking for the reopening of junior doctor positions, which received more than 57,000 signatures as of September.
The petition states that the multiple academic reforms and changes in the way they are assessed and graded negatively affected their results and mental health.
As a result, around 1,000 students chose to repeat their fourth and fifth year and 400 other students failed the competitive exam, the petition claims, adding that certain positions have also become more competitive.
"A student who wants to carry out a placement in Digestive Surgery in Paris must be ranked among the top 23% of his class, compared with 35% last year", the petition says.
It adds that consequently, many students will be compelled to choose a discipline which is easier to get into but they may not necessarily be invested in.
Medical student Marie warns some students would rather complete their studies abroad than give up on their ambitions.
She said she sees daily distress messages on Facebook support groups asking for advice on how fellow medical students can pursue their studies in Switzerland or Belgium.
To compensate, France might have to import foreign doctors in the opposite direction. "There may be a few more open positions for foreign practitioners who want to come and train in France," Hibon said.
However, French medical students see such a solution as unfair, both to them and the foreign doctors who may come in. "Foreign doctors are also being fooled because they are less paid than us, so they are also being exploited," Marie said.
More generally, the debate is taking place at a time when the whole medical sector in France is suffering from deteriorating mental health and working conditions — exhaustion, overtime, a lack of supervision, competition, important responsibilities and low wages — exacerbated by the COVID-19 pandemic.
All of these challenges have been bubbling for years across Europe, yet there may be hope on the horizon for the continent's hospitals by way of the Bucharest Declaration on the health and care workforce, which WHO Europe representatives adopted in 2023.
The declaration calls for political action to improve the recruitment and retention of health and care workers, improve health workforce supply mechanisms, optimise the workforce's performance and increase public investment in workforce education.
Yet it remains to be seen how countries will implement the declaration in practice, and regardless, the stakes are high: a doctor struggling with deteriorating working conditions will surely negatively impact the quality of care.
"When a caregiver is mistreated, we know 10 patients are mistreated after," Marie said.